PRP
- Dr. Jaime DeGuzman, DTCM, L.Ac

- Dec 27, 2025
- 4 min read
Platelet-Rich Plasma (PRP) is one of the newer add-on treatments used alongside IVF. While it is not offered by all fertility clinics, some clinics use PRP in an effort to improve egg quality or to help thicken the uterine lining before an embryo transfer.

Background
As of this writing, PRP is still considered an experimental treatment with mixed results. Most available evidence suggests potential benefits for women with repeated implantation failure and thin endometrium. There is even less reliable data for poor ovarian responders. Some studies indicate that intraovarian PRP injections may improve ovarian function, as reflected by increased antral follicle count (AFC) and anti-Müllerian hormone (AMH) levels, along with decreased follicle-stimulating hormone (FSH) levels.
Introduction
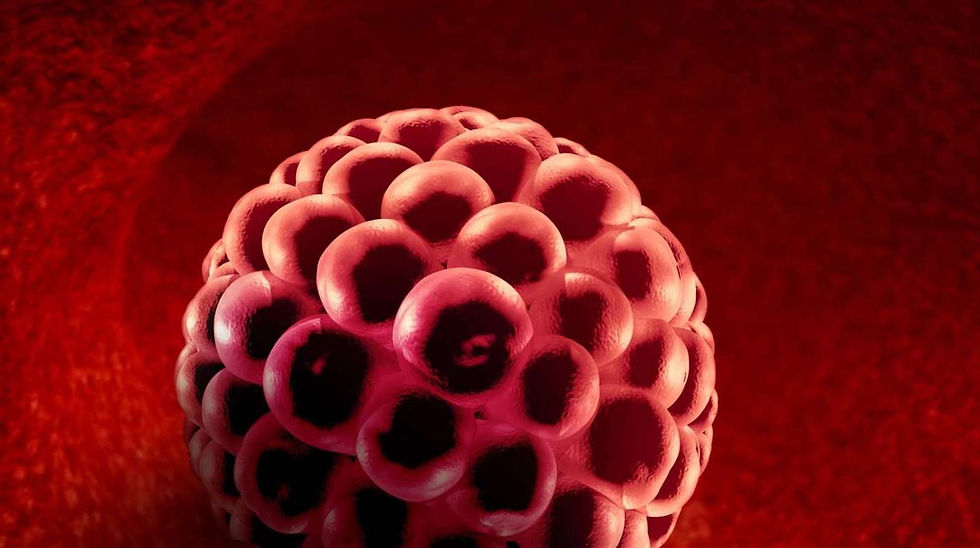
Poor egg quality is one of the most significant challenges in infertility treatment. PRP therapy offers a promising approach by injecting a concentrated solution of platelets—rich in powerful growth factors—directly into the ovaries, with the aim of enhancing egg quality. Using the same regenerative principles, PRP is also believed to improve the thickness of the uterine lining, addressing a common reason why embryo transfers are often cancelled.
Growth Factors
Growth factors are signaling proteins that promote healing, blood flow, cell growth, and tissue repair. PRP is created by drawing a small sample of a patient’s blood and spinning it in a centrifuge to concentrate the platelets, which contain these growth factors. The PRP is then injected into the ovaries or uterus with the goal of stimulating tissue repair and regeneration.
Intraovarian PRP
Using PRP for ovarian rejuvenation may be a promising option for women experiencing age-related fertility decline or certain conditions such as premature ovarian failure. A 2024 review published in Archives of Gynecology and Obstetrics looked at studies involving women with poor ovarian response and examined whether injecting PRP into the ovaries could improve hormone levels, egg supply markers, and outcomes of fertility treatments like IVF. The study concluded by saying that:
“ Intra-ovarian injection of PRP improved ovarian reserve markers with increasing AFC (antral follicular count), serum level of AMH(anti-Mullerian hormone) and day 3 estradiol and decreasing serum level of day 3 FSH (follicle-stimulating hormone).”
Another study looked at whether PRP could increase the number of mature eggs collected after ovarian stimulation in women aged 38 or younger with poor ovarian response who were undergoing IVF. The study analyzed 83 patients: 41 received PRP injections, while 42 did not receive any treatment. The results showed no significant difference in the number of eggs retrieved between the two groups. The study concluded by saying that:
“ Intraovarian PRP injection procedure does not improve mature oocyte yield after controlled ovarian stimulation (COS) in women less than 38 years old with an established IVF history of POR”
Intrauterine PRP
Researchers see promising potential for intrauterine PRP in women with repeated implantation failure (RIF) or a thin endometrium (less than 7 mm). For example, a retrospective study evaluating intrauterine PRP in patients with RIF found that PRP treatment was associated with higher β-hCG positivity rates, clinical pregnancy rates (CPR), and live birth rates (LBR) in women undergoing frozen embryo transfer (FET) cycles.
A meta analysis that looked at eight randomized control trials (RCTs) involving a total of 678 patients with thin endometrium (less than 7 mm), concluded that intrauterine PRP infusion may be an effective and safe treatment for women with thin endometrium. The study showed significantly better outcomes in patients who received PRP infusion compared with the control group. Improvements were seen in endometrial thickness, clinical pregnancy rate, live birth rate, embryo implantation rate, and a lower cycle cancellation rate.
“ Intrauterine PRP infusion may be an effective and safe treatment for women with thin endometrium.”
More Data and More Standardization Needed
Conflicting study results, the lack of large clinical trials, and the absence of standardized PRP protocols have made experts cautious about recommending this treatment for infertility. For example, a review published in Human Reproduction explains that PRP made from resting platelets differs significantly from PRP made with activated platelets, and that the method of activation affects which growth factors are released. Despite this, studies on ovarian rejuvenation use widely different PRP preparation methods. Some activate platelets with calcium or thrombin, others inject non-activated platelets, and many do not clearly describe their activation process.
TCM in Ovarian and Endometrium Health
Traditional Chinese medicine (TCM), particularly herbal formulas and acupuncture, has been used for thousands of years to support ovarian health in infertility treatment. TCM is thought to work by helping regulate hormone balance through the hypothalamic–pituitary–ovarian axis, reducing oxidative stress, and protecting ovarian cells from damage. A 2025 systematic review that analyzed studies from the past decade found that TCM interventions significantly increased anti-Müllerian hormone (AMH) levels, increased antral follicle count (AFC), and decreased follicle-stimulating hormone (FSH) levels in women with diminished ovarian reserve (DOR). The study concluded by saying that:
“ TCM exerts therapeutic advantages through multi-component synergistic effects, from improving the ovarian microenvironment, regulating reproductive endocrinology, delaying follicular atresia, etc. which provides a theoretical basis and practical reference for the integrated treatment of DOR.”
In addition, randomized and prospective studies have shown that TCM may help increase endometrial thickness and improve endometrial receptivity in women with infertility, particularly those with a thin endometrium. For example, a study published in Gynecological Endocrinology in 2023 examined the effectiveness of a traditional Chinese medicine formula, Zi Gui Nu Zhen, in treating infertility related to thin endometrium.The study concluded by saying:
“ In infertile women with thin endometrium who wish to conceive, two months' application of Zi Gui Nu Zhen can improve endometrial properties and proliferation, which is necessary for a healthy pregnancy, and increase the clinical pregnancy rate”
Conclusion
Even though there are contradictory findings and methodological limitations in most of the studies available and a lack of PRP standardization to draw firm conclusions about PRP’s effectiveness, there’s enough data to support that in the near future this technique will be more widely accepted. For now, most experts agree that PRP should be considered experimental until large, well-designed randomized controlled trials are completed.





Comments